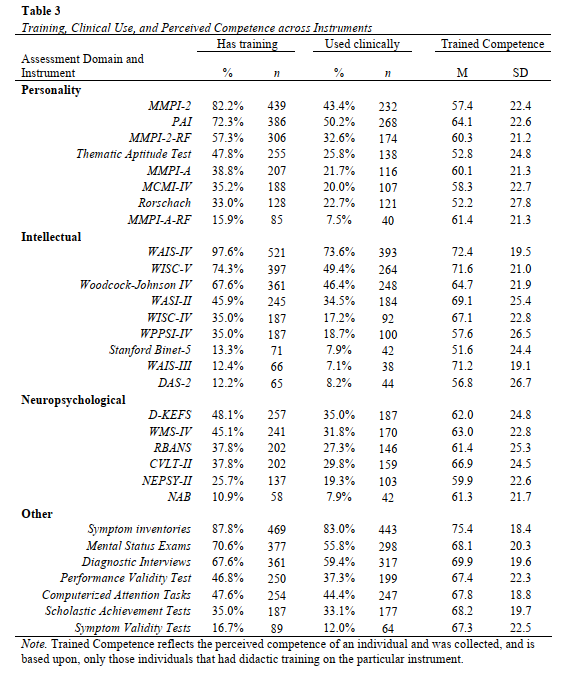
About a year and a half ago I launched (and subsequently published) a pilot project with Drs. Adam Schmidt and Matt Cribbet to look at some trends in training for psychological assessment by asking trainees themselves about their experiences. This week, the first paper from the large scale study that followed-up on that pilot based on the feedback we received was published in Training and Education in Professional Psychology (TEPP) in a new article, this time using a national sample of 534 doctoral trainees from across the country in health service psychology programs. GET THE PDF HERE
In short, our results suggest that (i) the patterns of training coverage mirror the instrument use patterns of psychologists who are currently in clinical practice, (ii) students receive more frequent didactic and classroom exposure during training than practice opportunities with clients, and that (iii) program types [PhD,PsyD] and program areas [Clinical, Counseling] are generally similar in their coverage. Lets break down what this means to me, as a researcher and professional working to ensure appropriate and effective psychological assessments.
- It’s good to see training conform to what professionals do, in general. This means that students will likely be ready to step into similar professional roles as those we currently see existing.
- Having the same content across programs means that in a way, the field has converged on what is the standard of content coverage. That doesn’t mean that all content is covered the same, or that all programs are equally good at training, but it is a good starting point for ensuring high levels of client care.
- There are some things that students don’t get a lot (or enough) training on. One is structured diagnostic interviewing with 25% of students not having training / or not knowing they were trained (which is just as bad). Another is with symptom validity testing. Response styles are a major part of ensuring appropriate interpretations are made, so not being prepared to assess invalid responding means not being ready to appropriately make diagnostic decisions with the aide of assessments. This is a huge issue for the VA, and for veterans since 50-70% produce invalid symptom response styles on the MMPI (Ingram et al., 2019), making sure that isn’t characterized is critical to what treatment recommendations come next. Good care starts at good training. Say it with me.
- Students get lots more classroom time than hands on learning, but hands on learning is when the complexity and nuance of this advanced integrative skill come into play. To advance training, there has to be more clinical use – not just class coverage.
There was a lot more to unpack from the article, but those were a few of my reflections. I’m looking forward to where we go next as a research team on this, and am excited to see the work related to performance-based competency and factors impacting use and intention to work with psychological assessment.